Lower back and sciatica pain is a common malady and data suggests that 80% of the adult population will experience back pain at some point in their lives. The causes which contribute to the development of such pain can vary significantly from person to person. During the treatment process narrowing down the cause of ones pain is the first step. Often doctors prescribe routine orthopedic tests and imaging studies to help in this process. Common findings during these tests, include:
- Tears of the muscle or tendon fibers (strains)
- Tears of the ligaments in the back (sprains)
- Muscular Spasm
- Disc bulging or herniation causing nerve root pain
- Osteoarthritis
- Spondylolisthesis: vertebrae of lower spine slips out of alignment
- Spinal Stenosis: narrowing of spinal canal due to the aging process
- Skeletal Irregularities: scoliosis (S-shape curve to the spine), kyphosis (forward rounding of the back)
Non mechanical causes of lower back pain include: Infections, tumors, abdominal aortic aneurysm, kidney stones, osteoporosis, endometriosis, fibromyalgia among others.
It is important then for the physician or therapist to rule out some of the more common causes of lower back pain from the uncommon.
Piriformis Syndrome
It is estimated that at least 6% of patients who are diagnosed as having low back pain actually have Piriformis Syndrome. 1 With misdiagnosis numbers that high it is worth investigating further. Let us take a closer look into where the piriformis is located anatomically and what its function is.
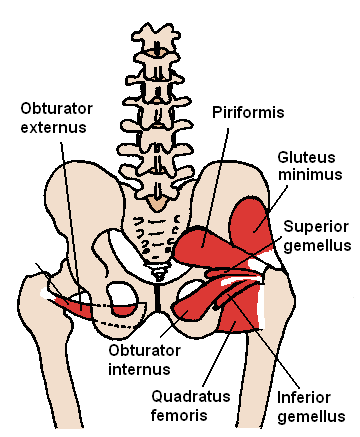
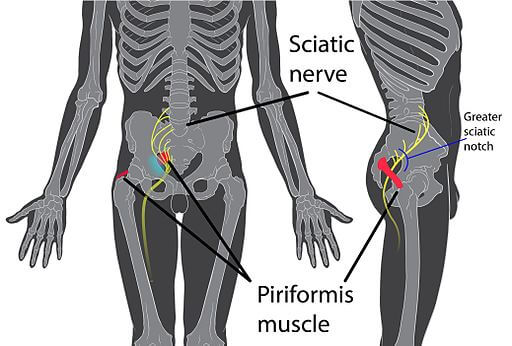
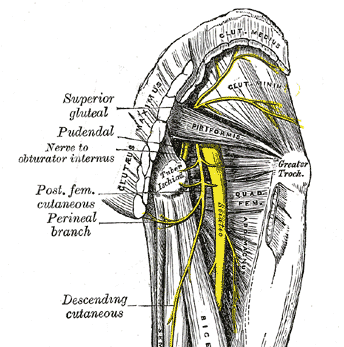
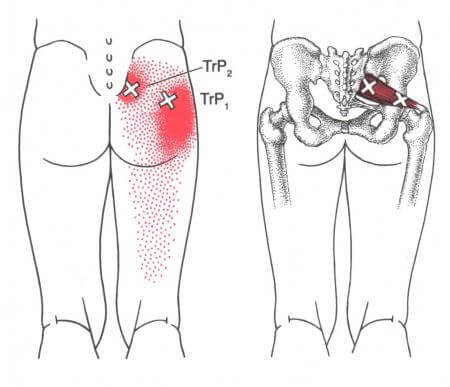
The piriformis is a muscle that originates from the bottom of the spine at the sacrum, spans underneath the buttock, and inserts at the top of the femur. Functionally this muscle rotates the hips in an outward motion away from the midline and also functions to spreads the legs apart.
Development of Piriformis Syndrome
As the result of a shortened, taught piriformis muscle or a lengthened and weakened one, the sciatic nerve situated underneath this muscle (and in approximately 10% of the population, directly through it) can become compressed. This can manifest symptoms such as dull or radiating pain in the lower back, buttock, and the posterior thigh that is usually increased by sitting, standing, and walking. 2
Situations which lead towards the development of Piriformis Syndrome include:
- Prolonged sitting and postural stress
- Trauma
- Abnormal spine alignment
- Pelvic tilt from previous surgery
- Uneven leg length
- Excessive exercise, such as running or climbing stairs
- Morton’s foot structure
How do I know if I have Piriformis Syndrome?
Diagnosis for Piriformis Syndrome is a diagnosis of exclusion. This means that only after diagnostic tests rule out more traditional causes such of pain, for example, nerve root compression, is a diagnoses of Piriformis Syndrome considered.
Specific tests include:
Freigberg Maneuver – The practitioner will ask the patient to lie face up with their leg extended and will rotate the leg towards the midline. This test attempts to stretch an irritated piriformis muscle to reproduce gluteal pain and or numbness down the extremity.
Straight Leg Test – Also face up, the practitioner will instruct the patient to flex their hip at a 90 degree angle and extend their knee straight out. By passively stretching in this position the practitioner is assessing the piriformis to see if this causes any pressure on the sciatic nerve.
Seated Piriformis Test – The patient should be seated in a chair with back upright and feet resting on the ground. The practitioner will place their hands on the outside of the knees and ask the patient to spread their knees apart while applying external force. Pain on the affected side would indicate a positive test.
Lastly, directly palpating trigger points that relate to the piriformis muscle may be helpful in diagnosis. These points typically lay at the lower border of the sacrum and around the posterior border of the hip joint.
Treatment
Treating Piriformis Syndrome involves correcting the perpetuating factors underlying the condition. Muscle pain does not exist within a vacuum and no one stretch will work for everybody. Most important in correcting the imbalance is figuring out if the piriformis really needs to be stretched or if it needs strengthening.
Stretching the piriformis
A simple test to determine if your piriformis needs to be stretched is to see how deeply your hip opens while seated and performing a figure four stretch. To test, sit down in a chair and flex the affected leg up towards your chest and rest the outside of your ankle over the thigh of your opposite leg. Notice any tightness, pain, or difficulty during this process. Compare your findings to the unaffected side to measure the difference.

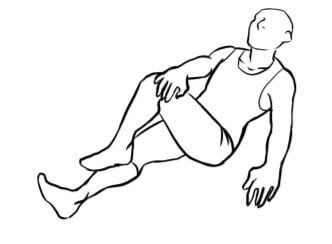
If upon stretching in the above manner reveals tightness consider additional daily at home stretches such as the one below. This can be performed by crossing the affected leg over the side of the opposite thigh and then by resting the opposite hand on the knee of the affected limb. For an additional stretch place your free hand on the affected hip and apply downward pressure towards the floor.
Strengthening the piriformis
As a muscle becomes overworked there is a tendency for the muscle to weaken and elongate. It would not be productive to further stretch and to elongate an already lengthened muscle as that would aggravate it further. In this instance, strengthening the weakened muscle would be the best option. Below are two options to strengthen a weakened piriformis muscle.
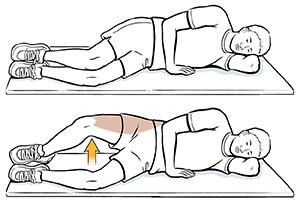
Perform the “clam shell” strengthening exercise by lying on your unaffected side and by placing your knees and feet together. Then start by separating your top knee from the bottom knee and rotating your hip away from the midline. Slowly return to the starting position. Repeat 10 times.
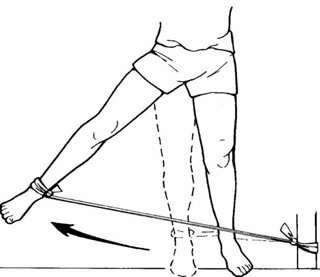
Further strengthening of the piriformis can be performed with or without the use of a TheraBand for increased resistance. To perform this movement simply stand upright with your feet shoulder width apart or by grasping with one hand onto a sturdy object such as a wall or chair. Raise the affected leg up away from the body, pause, and slowly return back to the neutral position. Repeat 10 times.
Additional considerations for weak hip abductors
Being mindful of the position of ones hips throughout the day can lessen the amount of strain and decrease further functional muscle imbalances, additional precautions to consider are:
- Not crossing the legs
- Limiting the amount of time spent seated
- Sitting or standing on one foot
- If a side sleeper, placing a pillow between legs as to limit further stretching of weakened muscle.
Modalities and Medical interventions
Methods of care that exist to alleviate the discomfort of Piriformis Syndrome and that can be combined with self care include:
- Physical Therapy
- Massage
- Acupuncture
- Injection, trigger point therapy
- Surgical intervention
- Heat and intermittent cold therapy
Source:
- The Journal of the American Osteopathic Association, November 2008, Vol. 108, 657-664.
- Simons, David G, Janet G. Travell, Lois S. Simons, and Janet G. Travell. Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual Volume 2, p. 186. Baltimore: Williams & Wilkins, 1999. Print.
- “Sciatica Stretches and Exercises”. April 2019, https://www.brownlowhealth.co.uk/wp-content/uploads/2019/04/sciatica-printable-pdf.pdf
- “Side lying hip adduction”. 3/29/2016, https://healthlibrary.uchicagomedicine.org/Content/healthsheets-v1/side-lying-hip-abduction-strength/
- “Hip abductor strengthening”. 2005, http://crh.marshall.edu/Resproj/2005/AFoy/Page%208.htm